By definition, sudden cardiac arrest seems to come out of nowhere. The most shocking cases are when young athletes collapse on the field, but this type of calamity also strikes dedicated middle-age runners, retirees whose health problems seemed well under control, adults of all ages and class.
If the person is lucky, medical help is close enough to get the heart beating again after it stops and before brain damage sets in, and the search for the hidden cause can begin. The less fortunate face terrible odds: survival rates for cardiac arrest outside a hospital have remained stuck at 10% for decades.
At last, researchers are making headway on a problem that kills more than 400,000 Americans every year. Genetic analysis is revealing new vulnerabilities and syndromes; painstaking field work has built the foundation for risk prediction tools; cell therapies are moving toward clinical trials. These efforts are laying a strategy for sudden cardiac arrest that doesn’t depend so heavily on luck.
Sudden cardiac arrest — when heartbeats, breathing, pulse, and blood circulation all halt — stems from problems with the electrical activity within the heart. Although in some people it can follow previously diagnosed heart disease, it’s not the same as a heart attack, when blocked blood vessels progressively rob the heart of oxygen and damage cardiac muscle. Sudden arrest has myriad causes: Coronary artery disease is a risk factor, as are congestive heart failure and structural problems in the heart or arteries present at birth or developed later. An irregular heart rhythm and its electrical chaos tilt the scales even more.
Frank Toro was lucky, or so he’s told. An 83-year-old Vietnam veteran from Thousands Oaks, Calif., Toro has to ask Bobbi, his wife of 61 years, to recount the whole story.
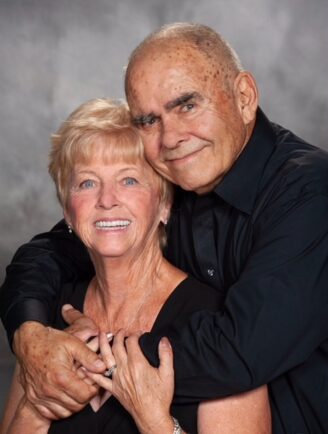
One day in 2012, he left his Southern California gym after lifting weights, climbed into his Ford 150 truck, drove a few blocks, and then crashed into a fire hydrant right before the eyes of two EMTs returning from a call. They leaped out of their ambulance and raced to his truck, opening the mercifully unlocked passenger door to bring him back to life with CPR and an external defibrillator.
What happened?
Toro remembers none of it, from the day before his heart stopped beating to more than a week later, when he was slowly brought out of therapeutic hypothermia and a coma induced to protect his brain. His strongest memory? “I couldn’t drive for three months,” he said of his return home. “That drove me nuts.”
At his side in the hospital, Bobbi knew he would be OK when he squeezed their son’s hand. “That was very touching, you know, because he knew who he was,” Bobbi said.
Frank Toro gets his medical care from the VA, which declared him disabled and eligible for benefits a few years ago because he was exposed to Agent Orange while serving in Vietnam. Like millions of other Americans, he has a family history of heart disease. His father died at age 59 and his grandfather succumbed to sudden cardiac arrest at age 64 while Frank was 6 or 7 years old, holding his hand at a movie theater. The Toros are reaching for answers.
“He’s very strong, very active. But he’s having some problems right now,” Bobbi said.
Still, the vast majority of people with heart disease do not ever experience sudden cardiac arrest.
No one knows exactly why Frank’s heart simply stopped beating.
‘A thousand Americans a day’
Back in 1970, researchers at the University of Michigan described the mystery of sudden cardiac arrest this way: “Although sudden deaths often seem to occur without warning, the victims are predisposed by conditions which are detectable long before the catastrophic event. The identification of conditions which are precursors of sudden death from coronary heart disease permits a rational consideration of possible preventive measures.”
If only.
“It affects a thousand Americans a day,” Sumeet Chugh, a cardiologist who specializes in electrophysiology research at Cedars-Sinai Medical Center’s Smidt Heart Institute, told STAT. “But if you look in the community it’s still rare. It’s not like high blood pressure or diabetes. It’s 50 people per 100,000 people.”
Extensive field work has led to lists of risk factors. These potential precursors have been compiled from large population studies, led by Chugh’s team in Ventura County, Calif., and Portland, Ore. The scale is necessary because cases are infrequent relative to other cardiovascular events. Their work needs to be tested in clinical trials.
Bystander CPR and automated external defibrillators help keep those numbers from being worse, but not all hearts can start beating again, and not all hearts can be shocked back into action.
There is a glimmer of hope in a procedure called extracorporeal CPR, which connects a patient to a machine that oxygenates blood, then sends it back through the body to restore circulation and keep organs from failing. It relies on a portable extracorporeal membrane oxygenation device, better known as the ECMO machine found in intensive care units, and it’s used in addition to standard CPR. ECPR also depends on the patient being at the right place at the right time to benefit from a sophisticated and scarce treatment.
Looking back to the 1990s, people with heart failure, a diagnosis that means the heart doesn’t pump blood throughout the body as well as it should, were shown to benefit from implantable cardioverter defibrillators. These ICDs detect abnormal rhythms and shock the heart back to normal within eight to 10 seconds rather than the eight to 10 minutes that might elapse before help could arrive in a best-case scenario. In addition, drugs have greatly improved for people with heart failure.
Despite those advances, it’s not enough to focus only on heart failure patients, Chugh said.
“This is still not preventing the cardiac arrest from happening, but it’s treating cardiac arrest immediately,” he said. “The defibrillators are only touching 30% of all people who are destined to have a cardiac arrest.”
Searching for early warning signs
It took 20 years, but Chugh’s group has come up with a risk prediction tool, published two years ago after following 2 million people in the California and Oregon studies. They were mindful that in general, for 40% of people, a cardiac arrest was their first sign of heart disease.
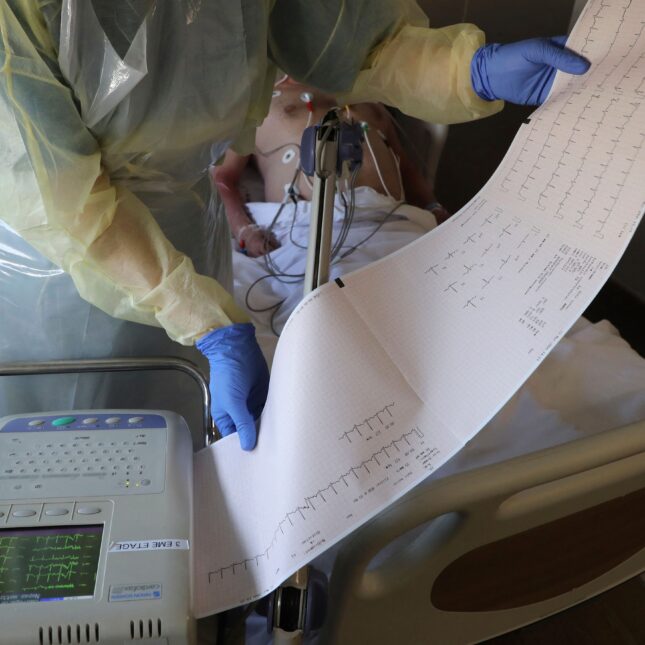
Enough of these participants shared 13 common elements to develop a precision tool, including markers of heart failure and diabetes as well as eight signatures on electrocardiograms and one on echocardiograms. These markers could become the basis for an early warning from doctors to patients at risk.
“We find that 60% of people under 35 who had a cardiac arrest had at least one traditional cardiovascular risk factor,” Chugh said. “The only way that you can make an impact is to nip it in the bud — predict it and prevent it before it happens.”
There’s another window of opportunity, up to two days or just hours before cardiac arrest. In the study, half of the 839 survivors in Oregon and half of the 823 ones in California had at least one warning symptom. But only 20% of them called 911 right away.
Those red flags could be all too familiar from heart attack signs people may also ignore: chest tightness, shortness of breath, weakness, fluttering or pounding heartbeats.
“The ones who called 911 right away had six-fold higher cardiac arrest survival compared to the ones that don’t,” Chugh said.
Less-immediate warning signs could be longstanding issues such as heart failure and diabetes also identified in the prediction tool, said Eric Stecker, an electrophysiologist at Oregon Health and Science University. “Because the person had a heart attack two years ago, or they have a cardiomyopathy where their heart is weak, those can predispose to primary arrhythmias that can lead to death without a heart attack.”
Sometimes electrocardiogram readings, also important in predictions, can warn of sudden cardiac arrest triggered by genetic predispositions for electrical abnormalities in the heart, such as longQT syndrome. “This is something that if you look at the EKG, you can see that there is a problem. The normal pattern of electrical impulses from the heart is altered,” Patrice Desvigne-Nickens, a physician-scientist at the National Heart, Lung, and Blood Institute, said regarding research on vigorous versus mild exercise in people who were given ICDs after heart rhythm problems were detected.
Chugh calls EKGs “the cheapest cardiac test in the world,” but researchers have set their sights on more sophisticated, precise methods, including cell therapies and genetic predictors of risk. “We’re not as close as you think, having really focused on genetics for decades, but we’ll get there,” he said.
Stecker also said tailored treatment will be important in future years. “But we’re not there yet.”
A genetic flaw tests couldn’t spot
In the realm of genetics, Canadian scientists recently discovered why some family members were so susceptible to sudden cardiac arrest. They shared a mutation in one gene, but that was not the whole story.
It begins with calcium release deficiency syndrome, a cause of sudden death recognized only in 2021. Its prevalence is unknown because the flawed intracellular mechanism can’t be picked up by the usual kind of testing conducted following unexplained fainting spells or a relative suffering sudden cardiac arrest.
It took the kind of genetic testing available in research labs to reveal that a genetic mutation can make the lower chambers of their hearts beat too quickly.
In 2016 Jason Roberts, a cardiologist and arrhythmia specialist at McMaster University in Ontario, Canada, encountered a family, many of whose members experienced sudden cardiac arrest. Unexplained fainting as well as their losses brought them to testing that proved fruitless. On electrocardiograms, ultrasounds, treadmill tests, and Holter monitors, everything appeared normal.
A deeper dive with more sensitive genetic methods found a one-letter change in a gene called RYR2, which codes for a cardiac-related receptor that can become overactive in a condition known as catecholaminergic polymorphic ventricular tachycardia, or CPVT.
“It’s relatively easy to diagnose if you look for it,” Roberts said. “If you put patients on a treadmill, they get lots of extra beats.”
Not that genetic flaw
But the family in question didn’t fit that picture. And more of them were dying, including a teenager who had been a track athlete in high school but two years later succumbed while running after her dog.
Roberts reached out to Wayne Chen, a professor at the University of Calgary whose lab focuses on calcium channels in heart disease as well as sudden cardiac death.
Together they discovered the RYR2 gene in this family was causing underactivity, not overactivity, in a new disease they named calcium release deficiency syndrome.
“When a young, otherwise healthy person dies, you really, really want, for the rest of the family, to be able to understand, because there’s nothing worse than having multiple other brothers and sisters and relatives continuing to die,” Roberts said. “And unfortunately, that’s been the case with CRDS.”
Roberts and Chen reported their findings in JAMA in June after studying 10 patients. It was a departure for the journal to publish a paper based on so few people and on animal experiments, but there was added urgency, editors explained in a note.
Roberts thinks they now have a relatively simple way to diagnose the syndrome, distinguishing between the two variants to see whether they are benign or serious and to gauge who would benefit from a pacemaker or an ICD.
The test involves provoking a signature wave on an electrocardiogram, while more research continues. “This could be incorporated into our routine for diagnosing other unexplained sudden deaths,” said Chen, who is working with mouse models.
Roberts is sanguine.
“We’re still in our infancy,” he said. “We just realized this is a syndrome.”
Helping hearts heal themselves
Cell-based therapies are also in their early days.
Eugenio Cingolani, director of cardiogenetics and preclinical research in the Smidt Heart Institute at Cedars-Sinai, has launched trials to give the heart a power it doesn’t have: the ability to grow new cells and repair damage that can lead to cardiac arrest.
ICDs respond to rhythm disturbances, but catheter ablation, in which abnormal heart tissue is destroyed, is another way to restore a healthy rhythm to the heart. There’s a downside: The complex procedure also damages healthy heart tissue, leaving scars.
Cingolani’s lab is about to test a cell-based therapy to treat a dangerous arrhythmia called ventricular tachycardia. Their approach delivers stem cell-derived exosomes — tiny fluid-filled sacs found inside cells — to heal heart scars.
“By shrinking that scar-affected inflammation and avoiding destroying nerve tissue, you prevent arrhythmia,” he said.
So far experiments have moved from cells to pigs. The next step is a first-in-human trial funded by the California Institute for Regenerative Medicine.
“A therapy like this potentially could be something that you could administer through a vein without having to have a super-specialized center doing it,” he said. “One of my additional motivations is having a therapy that could potentially reach a broader spectrum of the population and not only be given in specialized centers.”
‘Do you ever get over it?’
While the science advances, Bobbi Toro is focused on today. The Toros’ children have high blood pressure, she said, and one of them recently had a heart attack.
After her husband’s frightening experience, Bobbi is doing all she can to help others in her shoes. She teaches CPR in a group of patients and family members dedicated to recognizing trouble and performing bystander CPR if need be. When one cardiac arrest survivor witnessed someone have a cardiac arrest, he saved his life, she said.
That’s gratifying. Still, her life will never be the same.
“Do you ever get over it? I mean, it’s been 12 years,” she said. “I will tell you, even last night, he was very quiet while we were sleeping, and he was turned away from me. And I watch his body to make sure he’s breathing. Oh my God, I mean, I still do that.”
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies. Our financial supporters are not involved in any decisions about our journalism.
To submit a correction request, please visit our Contact Us page.











STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect