As a global health investor and public health advocate, I understand the benefit of weight loss drugs and the rush to promote Ozempic, Wegovy, and other GLP-1 drugs. What I cannot wrap my head around is how, almost 45 years after the World Health Organization announced that smallpox had been eradicated, the world is once again dealing with smallpox vaccines and treatments, this time aimed at mpox.
Mpox is a disease spread between animals and people that stems from the same virus family that causes smallpox. Mpox may be even more difficult, if not impossible, to eradicate because it can linger in nonhuman animals. It causes painful rashes, blisters, bumps and flu-like symptoms that last up to four weeks. If not detected in time and treated correctly, the disease can be highly disfiguring, or even fatal.
Mpox first emerged in West and Central Africa in 1970. In 2022, it began appearing in the United States, France, India, Australia, and other countries where it had not been seen before, driven by what’s known as the clade II variant. Although the outbreak faded away, a more dangerous variant known as clade I has since been spreading in the Democratic Republic of Congo and has recently reached neighboring countries. This variant has a 10% mortality rate, disproportionally affecting children under age 15, who account for 60% of mpox cases in the DRC.
With more than 14,000 cases and at least 511 deaths reported since the beginning of 2024, the World Health Organization has announced forming a panel to determine whether this outbreak should be considered a public health emergency of international concern. Additionally, the Africa Centres for Disease Control and Prevention said on August 8 that it will likely declare its first-ever public health emergency of continental security soon, after the disease has spread across six additional countries in only 10 days.
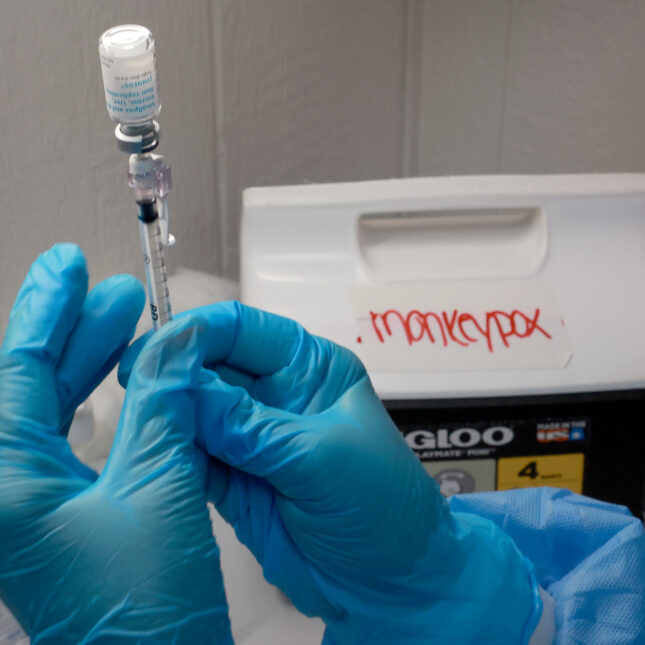
Vaccines and treatments are already available for the mpox virus. Animal studies and human antibody responses have shown that the JYNNEOS vaccine is likely a useful tool for preventing mpox, with recent effectiveness studies suggesting 66% to 89% protection. But the demand for mpox vaccinations does not have the same level of incentives as weight loss drugs, and far fewer resources have been invested in making the vaccine accessible globally.
Numerous bureaucratic and commercial challenges prevent making JYNNEOS more widely available at scale, including uncertain demand dynamics, cost, and public awareness. The same is true for TPOXX (tecovirimat), a treatment approved for smallpox infections that is assumed to be effective against mpox, but is currently only available off-label.
Despite the awareness of the potential global threat represented by mpox, instead of fighting against the disease when it was still confined to Africa, it was allowed to continue to grow exponentially and attack more people, until it came to the U.S. and other countries in 2022. Why did this happen? Didn’t the global community learn something from a pandemic that put the world into lockdown?
It might not be too late to stop mpox. There have been some positive steps toward implementing mpox vaccinations in Africa, with the DRC granting emergency use authorization for JYNNEOS and LC16, another smallpox vaccine made by KM Biologics, to address the growing threat of clade I. Gavi, an international organization that aims to increase vaccine access in low- and middle-income countries, intends to set up a stockpile for mpox vaccines, although this likely won’t be ready until 2026.
While programmatic efforts in the wake of an ongoing outbreak should be lauded, more proactive measures to invest in the development and manufacturing of new or improved vaccines and treatments is critical to ensure rapid response and global access, though these solutions may require a few years to fully scale. Recent initiatives from some industry partners make me hopeful that something may change in the future. Bavarian Nordic, the manufacturer behind JYNNEOS, donated 15,000 vaccine doses and recently announced a partnership with CEPI, while SIGA Technologies signed certain agreements to increase access to TPOXX.
These initiatives, however, are largely reactive and the global health community continues to scramble to address the increasing threat of mpox. Closer collaboration among the biopharmaceutical industry, funders, and international organizations is essential to galvanize a robust global outbreak response before it’s too late.
Further complicating the situation is the international regulatory framework. Until existing vaccines receive WHO prequalification — an important but often lengthy assessment process that certifies the safety and effectiveness of global health products procured by donor-funded agencies for developing countries — Gavi can rely only on donations of vaccines from the U.S. and Japan. So uncertainty prevails, and procurement remains slow.
Outbreaks like the current re-emergence of mpox are a reminder that global resources — including manufacturing and supportive policies — must be mobilized in time to prevent public health emergencies and reduce the risk of future pandemics. In the meantime, wealthy nations will likely continue their obsession with weight loss drugs, and drug manufacturers will continue to invest in them, often neglecting the threat of emerging infectious diseases.
Giulia Balconi, M.P.H., supports research efforts at Adjuvant Capital, an impact investment firm supporting life sciences technology companies focused on historically neglected diseases and maternal/child health.
LETTER TO THE EDITOR
Have an opinion on this essay? Submit a letter to the editor here.
To submit a correction request, please visit our Contact Us page.










STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect