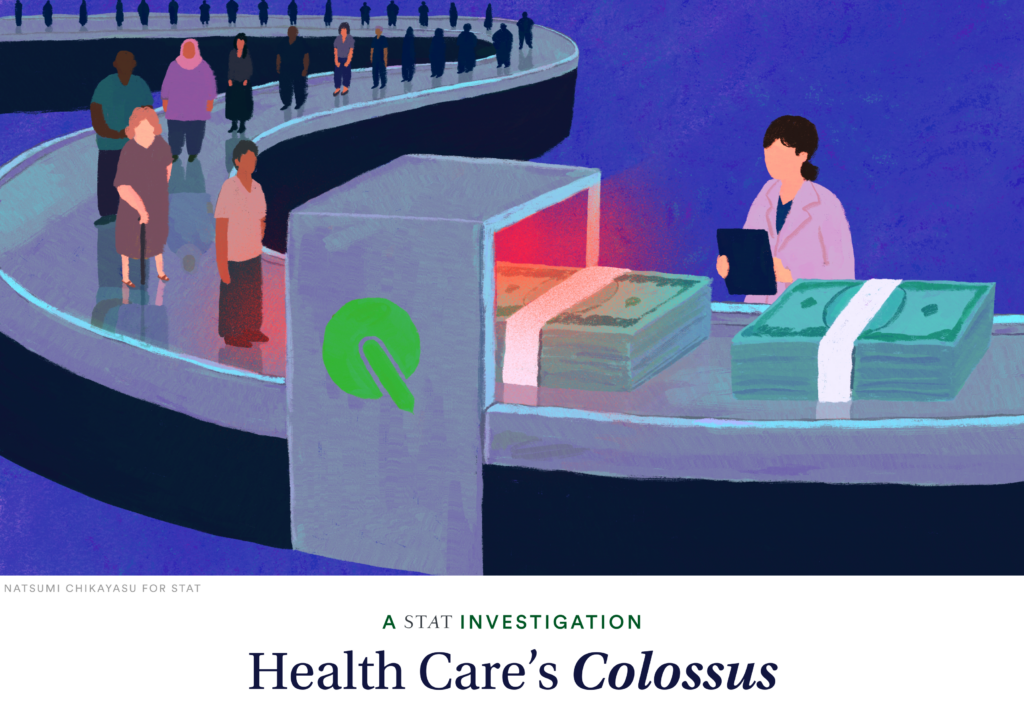
The nation’s largest health care company pressed thousands of its clinicians to use a thinly tested medical device to screen people for artery disease, dramatically boosting payments from the federal government for years even though many of the patients were not sick, a STAT investigation found.
The result was a torrent of sometimes questionable diagnoses of peripheral artery disease. Each one allowed the company, UnitedHealth Group, to claim thousands of dollars of extra payments tied to patients covered under Medicare Advantage, the increasingly popular version of Medicare run by private insurers. In many cases, those diagnoses were not medically useful, either because they were false positives or because they flagged early-stage disease, which isn’t typically treated, according to nine clinicians.
UnitedHealth was perfectly positioned to invent a national screening program and profit from it. Over the last two decades it has assembled an unrivaled collection of physicians — some 90,000 doctors in all — and used this empire to pad its bottom line, as STAT previously reported. At the same time, it has cemented its lead as the largest Medicare Advantage insurer. The full story of the company’s sweeping vascular disease screening program, detailed here for the first time, reveals how UnitedHealth has used its growing dominance across the health care system to its own benefit — and to the detriment of doctors, patients, and taxpayers.
This article is exclusive to STAT+ subscribers
Unlock this article — plus in-depth analysis, newsletters, premium events, and networking platform access.
Already have an account? Log in
Already have an account? Log in
To submit a correction request, please visit our Contact Us page.





STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect